Updated on Dec. 17, 2025
What is Myofascial Release (MFR)

Myofascial release (MFR) therapy is a massage technique that releases fascia tension. Accumulated unresolved fascial tension can develop into myofascial pain.
The myofascial release technique is the manipulation of soft tissue with a sustained and appropriate amount of pressure to release fascial adhesions and trigger points. A constant pressure is applied along the fascia's direction to stretch and lengthen the fascia, therefore breaking down the adhesion and trigger points.
With highly sensitive palpatory skills, the RMT applies deliberate and sustained pressure intending to release the fascial adhesion.
Here is a little explanation of what is fascia:
What is fascia?
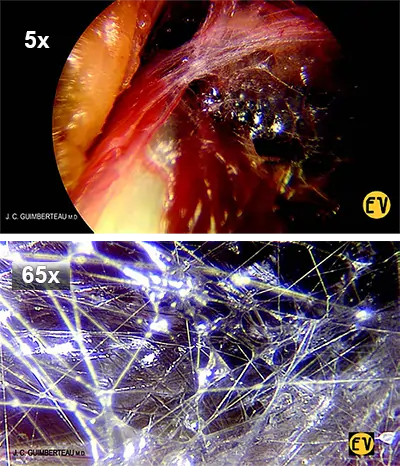
Fascia is a flexible/elastic tissue which permeates throughout our entire body. Unlike rigid bones, the network of fascia provides structure and shape to our body while being flexible, and bendable which allows us the freedom to move freely. Increasingly, there are more research studies on fascia. The definition of what is considered fascia has broadened.
Fascia: revised and broadened definition
The revised definition has broadened. An excerpt from the literature titled Anatomy, Fascia Layers, cited in PubMed stated that “.... Recently, the definition has been broadened to include all collagenous based soft tissues in the body, including cells that create and maintain the extracellular matrix. The new definition also includes certain tendons, ligaments, bursae, endomysium, perimysium, and epimysium. ....”
![Hierarchical structure of skeletal muscle. A) Sarcomere morphology and sliding mechanism (Scalebar 0.5 nm): Actin (red), Myosin (blue) and Titin (yellow) filaments are shown in the relaxed state (I) and during the contraction (II). The jagged sides represent the Z-lines. The central space without actin filaments is the H zone. B) Transmission Electron Microscopy (TEM) image of myofibrils (scalebar = 1 nm. Reproduced under CC0 1.0 Universal Public Domain Dedication. Author: Louisa Howard). C) Phase Contrast Microscope (PCM) image of skeletal muscle fibers. Dark violet elliptical elements are the myocytes nuclei (scalebar = 50 μm. Reproduced under CC0 1.0 Universal Public Domain Dedication. Author: Berkshire Community College). D) Histological image of a fascicle cross-section. Larger white bands are the perimysium membranes. Circular structures are the muscle fibers, while the darker violet dots are the myocytes nuclei (scalebar = 100 μm. Reproduced under Attribution-ShareAlike 3.0 Unported. Author: Ganimedes). E) Histological image of a portion of muscle cross-section. In the upper part, the epimysium membrane is visible (scalebar = 0.5 mm. adapted from [170] , reproduced under permission. Copyright 2008, Elsevier B.V.).](../../media/therapy/Hierarchical-structure-of-skeletal-muscle-A-Sarcomere-morphology-and-sliding-mechanism-400w_min.webp)
Reference: Hierarchical fibrous structures for muscle‐inspired soft‐actuators: A review - Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Hierarchical-structure-of-skeletal-muscle-A-Sarcomere-morphology-and-sliding-mechanism_fig1_343590590 [accessed 22 Nov 2024]
Fascia: the orange analogy explanation
If our bodies are like funky-looking oranges, not that we’re aspiring to be one! As with the orange, a membranous layer holds and wraps the juice into tiny sacs called the juice vesicles. Another thicker membrane wraps many of the juice vesicles into orange segments. The white layer wrapper beneath the peel, i.e. the pith, in turn, wraps the segments together within the rind or the peel into a whole fruit – the orange. In parallel to an orange, the fascia to our soft tissue muscle is the white layers of wrappers to the orange, and the material that forms our muscle is the juice of the orange.
So, fascia organizes and binds various tissues, muscles, and organs together so that they glide over each other smoothly. This is how our tissue and joints can move freely without any restrictions or pain … ~ … Only when the tissue is healthy. Our fascia becomes tight and knotted when the many layers of fascia are stuck together or stuck to the muscle. When this happens, we feel stiff or restricted in our movements, in more severe cases we may feel pain.
In short, like the mesh of blood vessels and the network of nerves, the fascia network permeates throughout the entire body.
As the fascial expert, Tom Myers has said, “….
You can just think of it like an orange. Each drop of juice is contained within one of those little cells. Those cells are contained within the section, that sections are contained within the pith and the pith is contained within the rind. “It’s the reason that the 60-70% of us that is made up of water isn’t a puddle on the ground.
What is myofascial pain syndrome?
Most people have muscle pain from time to time. However, the pain from myofascial pain syndrome is ongoing and longer-lasting. If left untreated, the pain is persistent and does not heal on its own.
Myofascial pain can also present itself as a trigger point. A trigger point is a hardened nodule of tight and contracted muscles. They are found anywhere in the body. However, the most common areas where trigger points can be found are the neck, back, and gluteal/buttock. A trigger point usually forms in the muscle belly and fascia of the muscles.
Symptoms of myofascial pain or trigger point:
- Pain over prolong period of time
- When applying physical pressure to the trigger point it can be painful. You may feel the hardened nodule or taut band twitches or “jumps” when touched.
- Referred pain; for example, a trigger point or “knot” in the neck can cause pain that spreads and tracks along the arm to the hand.
- Loss of strength in affected area. For example, with a trigger point or myofascial pain in the shoulder, you may find that it is very challenging to lift your arm to comb your hair.
- Restricted movement therefore, reducing function and mobility
What causes myofascial pain?
For many reasons, fascia can become tight and develop into painful trigger points if unaddressed. The cause of the trigger point is not clearly understood. According to a review article published in 2014 (MS Jafri), muscle trauma, muscle overuse and psychological stress are believed to result in myofascial trigger points.
Examples of common activities which can result in myofascial trigger points are:
- Muscle overload from activities such as lifting heavy loads at worksites or during performance activities of daily living tasks,
- Repetitive tasks – doing the same movement over and over for prolonged durations. Sitting for long periods looking over devices, working at laptops or computers or seated while driving for extended periods are considered repetitive tasks.
In the above examples, poor ergonomics, improper posture, de-conditioned muscle, and fatigue have been the common factors contributing to trigger point development. The article further indicated that elite athletes too, can develop myofascial trigger points. Although muscle conditioning has been shown to prevent trigger point development, activities which overexert above a certain threshold will incite the formation of trigger points.
Psychological and emotional stress can initiate the formation of trigger points. Being in a sustained stressful circumstance increases activation of the sympathetic nervous system i.e., the “fight or flight” response. The environment increases the susceptibility to developing trigger points
Can you prevent myofascial pain?
The onset of myofascial pain can be minimized. Healthy lifestyle habits are key to minimizing the risk of getting myofascial pain. We will need to keep our fascia healthy and supple by following the following:
- Get enough good quality sleep
- Eat a balanced diet, as much as possible avoid junk food
- Stay hydrated
- Minimize stress level
- Exercise and stretch regularly, my recommendation: A well-balanced, multi-planar movements type of physical activity
- Avoid physical injury, you may be in the gym weight training, or holding a prolonged posture during occupational activities causing overuse syndrome, e.g., sitting at the desk with your head and back hunched over devices and laptops.
Profile summary: Kin Sze, RMT
Kin Sze is a registered massage therapist in good standing with the College of Massage Therapists of Ontario (CMTO). He is also a certified fascial stretch therapist.
RMT sessions with Kin Sze are covered under work-extended health benefits.
He maintains his clinical practice at 2 locations in downtown Toronto:
b-Stretched - Queen West and Step Up Massage and Rehab - Adelaide
References: [click]
- Jafri, M. Saleet, Mechanisms of Myofascial Pain, International Scholarly Research Notices, 2014, 523924, 16 pages, 2014. https://doi.org/10.1155/2014/523924
- Langevin, Helene, M.D., Stretching, Connective Tissue, Chronic Pain, and Cancer - 2016 Kanbar Lecture on Innovations in Integrative Medicine, Integrative Medicine Today, UCSF Osher Center for Integrative Medicine, University of California Television, available on: https://www.uctv.tv/shows/Stretching-Connective-Tissue-Chronic-Pain-and-Cancer-2016-Kanbar-Lecture-on-Innovations-in-Integrative-Medicine-30714 and on YouTube: https://youtu.be/7Gcl7BN6-38?si=sk6ZU8mIHEUH15rn
- Chronic Myofascial Pain. myhealth.alberta.ca/Health/pages/conditions.aspx?hwid=uz2319
- Dave HD, Shook M, Varacallo MA. Anatomy, Skeletal Muscle. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537236/
- Bordoni B, Sugumar K, Varacallo MA. Myofascial Pain. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535344/
- M.S. Ajimsha, Noora R. Al-Mudahka, J.A. Al-Madzhar, Effectiveness of myofascial release: Systematic review of randomized controlled trials, Journal of Bodywork and Movement Therapies, Volume 19, Issue 1, 2015, Pages 102-112, ISSN 1360-8592, (https://www.sciencedirect.com/science/article/pii/S1360859214000862) available on: https://doi.org/10.1016/j.jbmt.2014.06.001
- Lea Overmann ∙ Robert Schleip ∙ Dennis Anheyer ∙ Johannes Michalak, Effectiveness of myofascial release for adults with chronic neck pain: a meta-analysis, Physiotherapy Journal, Volume 123, p 56-68, June 2024, available on: https://www.physiotherapyjournal.com/article/S0031-9406(23)00083-4/fulltext or (https://www.sciencedirect.com/science/article/pii/S1360859214000862)
- Tantanatip A, Chang KV. Myofascial Pain Syndrome. [Updated 2023 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499882/ Myofascial Pain Syndrome - StatPearls - NCBI Bookshelf
- Gatt A, Agarwal S, Zito PM. Anatomy, Fascia Layers. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526038/
You may be interested in:
Your Pain Is Personal to Me: How My Own Injury Led Me to Becoming RMT

A personal narrative from Registered Massage Therapist Kin Sze about how his own hamstring injury and career transition from engineering to massage therapy inform his empathetic, whole-body approach to treating neck and shoulder pain in Toronto.
